CHOLERA IN CHILDREN:
A CLINICAL OVERVIEW FOR MEDICAL PRACTITIONERS
Table of Contents
INTRODUCTION
Cholera is a dehydrating acute diarrhoeal disease with high levels of mortality if treatment is not immediately instituted. An estimated 1-4 million cases and 95,000 deaths are reported annually. Cholera is characterised with periodic outbreaks, as currently being witnessed in Nigeria, and reemergence as currently being experienced in war zones like Haiti and Yemen.
AETIOLOGY
Cholera is caused by Vibrio cholera, a gram negative, comma shaped rod. It is divided into serogroups by its somatic O antigen. There are > 200 serogroups but only O1 (subdivided into classical & El Tor) and O139 (no longer a major cause) cause epidemics
EPIDEMIOLOGY
Cholera primarily occurs in the settings of inadequate access to clean water and sanitation. Large epidemics often occur in the settings of natural disaster and conflict. It is common in resource-scarce environment.
Cholera occurs endemically (having reported cholera cases in at least 3 of the 5 past years) and epidemically primarily in Africa and Asia. Greater 90% of global cases now occur in Africa. Cases in resource-abundant setting are generally imported from endemic and epidemic settings
Humans are the only known host for the causative agent, V. cholerae. The organism thrives best in moderately salty water. It can also survive in nutrient-rich fresh water as occurs when there is organic pollution of water such as human faeces.
Ingestion of contaminated water and under-cooked shellfish are the main modes of transmission.
Host-based risk factors include age<2 years, blood group O, hypochlorhydria, partial gastrectomy, malnutrition, previous non-exposure, household contact of the infected.
PATHOGENESIS
Vibrio cholerae is transmitted via the faecal-oral route. Large inocula of bacteria (>108 CFU) are required. Smaller inocula (105 CFU) is required in persons whose gastric barriers are disrupted.
For infection to occur, V. cholerae must survive the acidic environment of the stomach, then attach to the small intestine and produce cholera toxin. The toxin activates an intracellular pathway resulting in massive fluid secretion into the small intestine that contain high concentration of Na, Cl, HCO3, and K
CLINICAL MANIFESTATION
Most cases are mild or inapparent. In symptomatic cases, 20% develop severe dehydration (fig 1). Incubation period: 1-2 days (hours to 5 days).
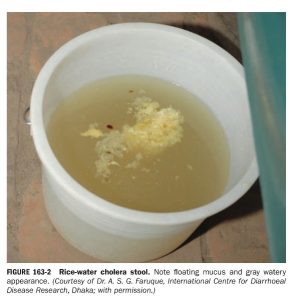
GIT: clear watery vomiting before or after diarrhoea; In early illness, stool contains fecal matter and bile. Fever and frank abdominal pain are uncommon. In severe cholera (cholera gravis), the stool is profuse (10-20ml/kg/hr), painless, tenesmus-free, rice-water stool (suspended flecks of mucus) with fishy smell (fig 2). In cholera sicca, there is rapid fluid loss confined to the intestinal lumen but no frank diarrhoea
MSS: muscle cramping and weakness (hypokalemia and hypocalcemia)
(fig 1): A Nigerian child with cholera and severe dehydration
Fig 2: rice-water stool
LABOARTORY FINDINGS
Features of dehydration which is usually isonatremic (Raised specific gravity & hemoconcentraion); others are: low serum K, Ca, glucose, HCO3; due to hemoconcentarion, high serum Na & Ca may be seen
COMPLICATION
The most common is hypovolemia and dyselectrolytaemia. Aspiration pneumonitis. Chronic enteropathy and malnutrition. Bacteremia is rare
DIAGNOSIS
- When to suspect cholera (WHO)
- In areas where cholera outbreak has not been declared: any person ≥ 2 years with acute watery diarrhoea (AWD)
- Once there’s cholera outbreak: any person with acute watery diarrhoea
- Gold standard for diagnosis: microbiologic isolation of V. cholerae ( stool, vomitus, rectal swab). The transport medium is Cary-Blair while selective medium (Thiosulfate-citrate-bile salt sucrose agar) is used. (confirmation is not required before treatment)
- Rapid diagnostic test are available and are highly sensitive and specific.
- Molecular identification using PCR exists
- Dark-filed microscopy: rapid identification of typical darting motility in wet mounts of rice-water stools
TREATMENT
Rehydration is the mainstay of therapy. Rice-based ORS is preferred to standard ORS and used for mild or moderate dehydration. Severe dehydration requires ringers lactate IVF. Fluid deficit should be replaced within 4 hours. Ongoing loss should be replaced. Frequent but small feeds should continue.
Single-dose per oral therapy is recommended and includes; doxycycline (2-4mg/kg; max 300mg), azithromycin (20mg/kg; max 1g), ciprofloxacin (20mg/kg; max 1g)
Zinc (10mg for <6 month of age; 20mg for > 6 months of age) is recommended
PREVENTION
The mainstay of cholera control are improved personal hygiene, access to clean water and sanitation. Raw or undercooked fish and shellfish should be avoided in cholera endemic region. Oral cholera vaccine provides protection for 2-5 years.